Credentialing Timeline

Credentialing Timeline
Credentialing Timeline
Becoming a credentialed provider is a lengthy and complex process. The timeline for credentialing differs depending on the payer. When you send applications to become an in-network provider, submit paperwork quickly for a faster process. Internal processes also need to take place to credential you properly. Government insurance plans like Medicaid and Medicare have a more rigorous process than private insurers like BCBS and Cigna. This is because of the additional liability government plans assume regarding their patients. Verification of each provider and practice is thorough to ensure that only qualified providers join the network.

A provider interest form must be sent to the insurance provider.
You should receive a response from the insurance provider in 10–15 days indicating whether they are accepting new practitioners in your area.
Submit an application if the network is open.
A committee meets monthly, though the meeting day varies by payer. If required documentation is missing by the committee meeting date, your application will be moved to the next meeting. With all documents in place, they will give you an answer within 30–45 days.
Application accepted or denied.
If approved, they will assign you an activation date.
Example: If the application is accepted on July 1st, they may assign an activation date for sometime in August.
The process still isn’t complete. Even after assigning the activation date, additional internal filing must be done to fully integrate the new provider into all associated networks.
The internal filing process begins.
They file and send your information to all associated plans and alert their customer service department of a new provider. This allows patients to recognize you as an in-network provider. This internal process can take up to 90 days. Full integration may take additional weeks before you can see patients and bill for services.
Expect the credentialing process to take 120–140 days.
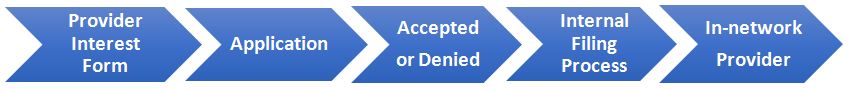
The entire credentialing process can span 120–140 days, from obtaining credentials to full integration across all payer networks.
Facing credentialing challenges? Call us for expert support today!
By: Riley Roberts, Healthcare Sales Representative
Recent Posts
- Optimizing PA Practice: State Rules for Provider Credentialing | TriumpHealth
- 2025 MIPS Targeted Review – Step By Step Guide to Maximize Incentives | TriumpHealth
- Overcoming Credentialing & Billing Challenges for Eye Surgeons & Eye Care Centers | TriumpHealth
- Why Timely MIPS Reporting Matters in 2025 | TriumpHealth
- Overcoming MIPS Reporting Challenges in Skilled Nursing Facilities (SNFs): A Guide for Success | TriumpHealth
- Maximizing ASC Billing Success: Guide for Plastic Surgery Practices | TriumpHealth


