Medical Billing &
Revenue Cycle
Management
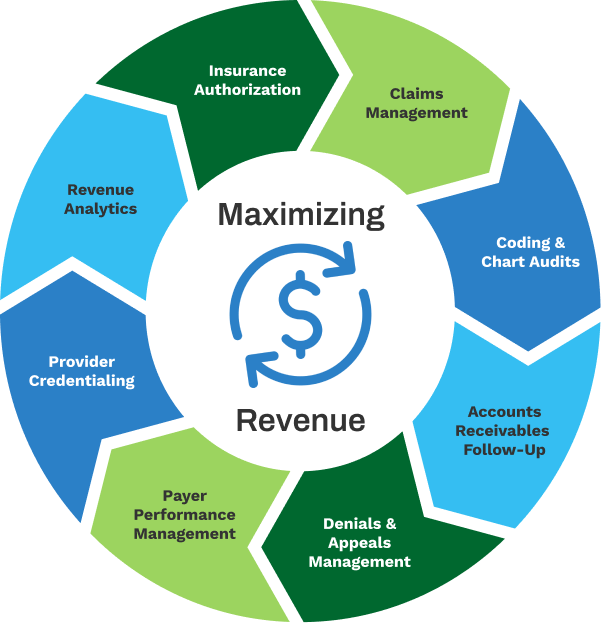
- Prior-Authorization
- Charge Entry & Claims Management
- Clinical Chart & Coding Audits
- Payment Posting
- Accounts Receivables Management
- Self-Pay Collections
- Denial Prevention
- Denial & Appeals Management
- Patient Statements & Patient Calls
- Provider Credentialing & Enrollment
- Practice Start-Up
- Financial Reporting & Analysis
Eliminate The Risks By Using Our Revenue Cycle Services!
The growing complexity of payer requirements and mandates has made it extremely challenging for healthcare organizations to capture revenue. Protecting your organization from lost revenue and high overhead expenses requires proactive revenue cycle management, real-time reimbursement analysis, and resolution of root causes for denied claims. You need fully comprehensive healthcare revenue cycle management run by professionals for the smooth delivery of the services.
What Is Healthcare Revenue Cycle Management (RCM)?
Revenue cycle management (RCM) refers to the process of managing and optimizing the financial aspects of a healthcare organization’s revenue cycle, starting from the initial patient encounter to the final reimbursement of services provided. It encompasses all the administrative and clinical functions related to billing, claims processing, payment collection, and revenue generation. The primary goal of revenue cycle management is to ensure timely and accurate reimbursement while maximizing revenue for the healthcare organization.
Effective revenue cycle management helps healthcare organizations streamline billing operations, minimize claim denials, optimize reimbursement, and improve overall financial performance. It requires a combination of skilled staff, efficient processes, up-to-date technology, and continuous monitoring and improvement to ensure a smooth and efficient revenue cycle.
Frequently Asked Questions
What is Medical Billing, and how does it contribute to the revenue cycle in healthcare?
Medical Billing involves the submission and management of claims to insurance companies for reimbursement of healthcare services provided. It contributes to the revenue cycle by facilitating the timely collection of payments, thus ensuring financial stability for the healthcare organizations.
How can outsourcing Medical Billing and Revenue Cycle Management benefit healthcare providers?
Outsourcing Medical Billing and Revenue Cycle Management can benefit healthcare providers by reducing administrative burden, improving billing accuracy, and ensuring compliance with regulations. This can lead to increased revenue and efficiency for medical practices.
What are the key components of Revenue Cycle Management, and how do they impact the financial health of a medical practice?
The key components of Revenue Cycle Management include patient registration, charge capture, claims submission, payment posting, and denial management. These processes directly impact the financial health of a medical practice by optimizing revenue collection and minimizing revenue leakage.
How do you ensure compliance with changing healthcare regulations and coding standards in Medical Billing?
Compliance with changing healthcare regulations and coding standards in Medical Billing is ensured through regular training, staying up to date with industry changes, and employing certified coding professionals. This helps healthcare providers avoid penalties and maintain billing accuracy.
Can you explain the importance of accurate coding in the Medical Billing process and its impact on reimbursement?
Accurate coding is essential in the Medical Billing process as it directly affects reimbursement rates, minimizes claim denials, and ensures compliance with insurance guidelines. By assigning the correct codes for procedures and diagnoses, healthcare providers can maximize revenue and avoid costly billing errors.
Advantages Of Using TriumpHealth Revenue Cycle
Management Services
TriumpHealth is an AI-driven healthcare revenue cycle management company that manages all denials, handles appeals, and follows-up on all outstanding claims to ensure payment in a timely manner. Our highly trained billing, coding, and denial management staff, plus leading technology and meticulous compliance processes will free you to focus on providing quality medical care and improved patient satisfaction. Our professional medical billing and healthcare revenue cycle services include:
What Makes Revenue Cycle
Management Services Different?
TriumpHealth helps you reduce costs and maximize reimbursement by:
-
-
-
-
-

Advanced Technology
Leverage cutting-edge tools for efficient and accurate medical billing.

Industry Expertise
Benefit from our team’s in-depth knowledge of payer rules and guidelines

Personalized Solutions
Tailored approaches to meet the unique needs of your medical practice.

Seamless Workflows
Experience smooth and efficient processes for optimal results.

Superior Results
Achieve excellence in medical billing with our proven track record of success.

Revenue Cycle Assessment
Optimal revenue cycle performance hinges on monitoring key performance indicators (KPIs).
Maximize Your Revenue. Schedule a Consultation Today!
We will help you achieve financial and regulatory compliance goals resulting in improved patient outcomes and increased revenue.














