MIPS 2020 Final Rule & Future Planning
MIPS 2020 Final Rule & Future Planning
MIPS 2020 Final Rule & Future Planning
The Centers for Medicare and Medicaid Services (CMS) has released the Final Rule for the 2020 MIPS program. This Final Rule gradually increases MIPS reporting requirements and financial impact. Here, we highlight the most relevant changes for your 2020 MIPS performance. With these insights, you can better plan for future compliance.
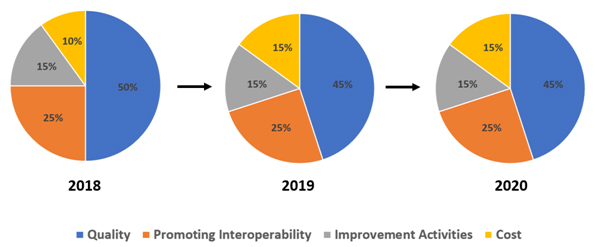
MIPS Performance Categories
In 2020, the MIPS category weights remain the same as in 2019.
2020 MIPS Categories
|
Quality |
Promoting Interoperability |
Improvement Activities |
Cost |
|---|---|---|---|
|
45% |
25% |
15% |
15% |
MIPS Reimbursement Overview
The 2020 performance year offers larger incentives due to higher thresholds and program changes. Clinicians who prioritize the program will see increased revenue. However, those who meet only the minimum requirements may face challenges. They could also encounter higher penalties in the future.
The lookback period is two years. Prepare in 2020 for payment adjustment in 2022.
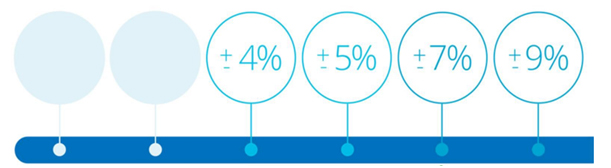
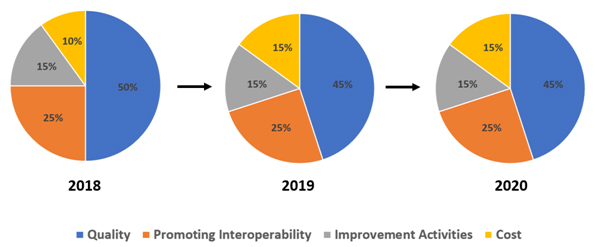
Performance Threshold & Financial Impact
In 2020, CMS increased the minimum performance and the exceptional bonus thresholds. Additionally, there will be more significant financial implications for MIPS-eligible clinicians who choose not to report.
| 2019 | 2020 |
| 30-point performance threshold | 45-point performance threshold |
| 75-point exceptional performance threshold | 85-point exceptional performance threshold |
| Maximum payment penalty set at -7% | Maximum payment penalty set at -9% |
| Maximum incentive prediction at +4.69% | Maximum incentive prediction at +6.25% |
Note: To ensure budget neutrality, positive payment adjustment is likely to be increased or decreased by an amount called a “scaling factor.” The amount of the scaling factor depends on the distribution of final scores across all MIPS-eligible clinicians.
MIPS Timeline
Below are pertinent milestones for the MIPS program.
| Milestone | Date |
| 2018 Performance Adjustment | Jan 1 – Dec 31, 2020 |
| 2019 Data Submission | March 31, 2020 |
| 2019 Performance Feedback | July 1, 2020 |
| 2019 Target Review | August 31, 2020 |
| 2020 Data Reporting | Jan 1 – Dec 31, 2020 |
| 2020 Performance Adjustment | Jan 1 – Dec 31, 2022 |
MIPS Eligible Clinicians
In 2020, the MIPS-eligible clinician categories remain the same as in 2019.
| 2020 MIPS Eligible Clinicians | |
| Physicians | Audiologists |
| Physician Assistants | Physical Therapists |
| Nurse Practitioners | Occupational Therapists |
| Clinical Nurse Specialists | Speech-Language Pathologists |
| Certified Registered Nurse Anesthetists | Clinical Psychologists |
| Audiologists | Registered Dieticians or Nutrition Professionals |
MIPS Eligibility Criteria
To be eligible to participate, the clinician must meet the following three requirements:
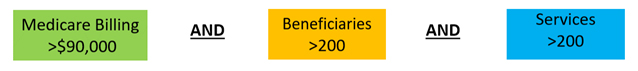 MIPS-eligible clinicians excluded due to low-volume threshold determination can opt into MIPS.
MIPS-eligible clinicians excluded due to low-volume threshold determination can opt into MIPS.
- If you’re an eligible clinician and meet at least one low-volume threshold criterion, you may opt into MIPS. To qualify, ensure you meet or exceed one criterion, even if you don’t meet them all.
- If you opt-in, you’ll be subject to the MIPS performance requirements, MIPS payment adjustment, etc.
Note: You can voluntarily report if you are a clinician or group not MIPS eligible. If you report voluntarily, you will receive an MIPS final score but no payment adjustment.
MIPS Performance Period
The performance periods for respective MIPS categories remain unchanged.
| Performance Category | 2019 | 2020 |
| Quality | 12 months | 12 months |
| Cost | 12 months | 12 months |
| Promoting Interoperability | 90 days | 90 days |
| Improvement Activities | 90 days | 90 days |
Changes in Quality
In 2020, expect the following changes in the Quality category:
- CMS removed 42 quality measures and added four new ones.
- The data completeness requirement rose from 60% to 70%. Now, you must report Quality measures on at least 70% of eligible cases, both Medicare and non-Medicare, annually.
- Measures not meeting the data completeness threshold will receive 0 points (previously 1 point in 2019).
- Small practice clinicians (15 or fewer in the TIN) will still earn 3 points for measures below the data completeness threshold.
- Several Quality measures have reached their limit or been removed.
- CMS has introduced new specialty sets for speech-language pathology, audiology, social work, chiropractic medicine, pulmonary care, nutrition/dietetics, and endocrinology.
- Flat percentage benchmarks are now in place for cases where CMS finds a benchmark may risk incentivizing inappropriate treatment for certain patients.
Changes in Promoting Interoperability (PI)
The PI category will not see any significant changes in 2020, except below:
- A group will be considered hospital-based and eligible for reweighting if more than 75% of the clinicians in the group meet the definition of a hospital-based individual MIPS-eligible clinician (it is currently 100%).
- CMS will remove the Verify Opioid Treatment Agreement measure and keep the Query of PDMP measure optional.
- Clinicians will be allowed to satisfy the optional Query of Prescription Drug Monitoring Program (PDMP) measure with a yes/no response instead of a numerator/denominator (also applies in 2019).
- The points for Support Electronic Referral Loops by Sending Health Information measure will be redistributed to Provide Patients Access to Their Health Information measure if an exclusion is claimed (also applies in 2019).
Changes in Improvement Categories (IA)
As with Quality measures, there is a net reduction in the number of IA measures. Here are the key changes:
- 15 IA activities were removed, two new ones added, and seven modified.
- CMS increased the participation threshold for group reporting from a single clinician to 50% of the clinicians in the practice.
- The definition of rural area was modified to mean a ZIP code designated as rural by the Federal Office of Rural Health Policy (FORHP) using the most recent FORHP Eligible ZIP Code file available.
Changes in Cost
The Cost category will see the most changes out of the four MIPS categories. Key changes are below:
- CMS is revising the current measures, such as the Medicare Spending Per Beneficiary Clinician and Total Per Capita Cost measures. There will be no changes to current case minimum requirements.
- The driver for the above change is to address the concern from clinicians of certain specialties that patients were attributed to them over whom they have minimal control, both regarding their behavior and clinical outcome. This negatively impacted the Cost score of the specialist clinician. The 2020 changes in patient attribution methodologies are expected to affect the cost score for the impacted clinicians positively.
- Ten new episode-based measures have been introduced, increasing the total number of such measures to 18.
MIPS Value Pathways (MVP)
To reduce the MIPS reporting burden on clinicians, CMS is adopting a new framework, which began in 2021 for performance year, called the MIPS Value Pathways. (MVPs) Under MVPs, clinicians would report on a smaller set of specialty-specific measures, outcome-based, and more closely aligned to Alternative Payment Models (APMs). MVPs aim to reduce the reporting burden by moving towards an aligned set of measures more relevant to a clinician’s scope of practice across all MIPS categories for different specialties or conditions.
Here is a CMS video explaining the MIPS Value Pathways framework. (Source https://qpp.cms.gov/mips/mips-value-pathways)
Planning for 2020
MIPS-eligible clinicians and groups should stay on top of their 2019 MIPS data reporting and simultaneously become familiar with the changes for MIPS in 2020. The 2020 final rule establishes higher performance thresholds and payment adjustments, so more planning and reporting will be necessary to avoid penalties.
TriumpHealth consultants help you acquire pertinent MIPS knowledge and plan and monitor performance. To see how we can help you maximize incentives, please click here or call us at (888) 747-3836 x1.
By Tej Gill – VP Healthcare Solutions, TriumpHealth
References:
Disclaimer:
The content provided by TriumpHealth is for informational purposes only and does not constitute legal, medical, or financial advice. Regulations and payer requirements may change; please consult a qualified professional for guidance specific to your situation. Click here to review our full legal disclaimer.
Recent Posts
- MIPS 2026 Updates: A Practical Guide for Clinicians, Practices, and Office Managers
- CHAP Accreditation Updates for DME Suppliers: Step-by-Step Guide for Location Changes and Adding New DME Supplies
- Payer Contract Negotiations: Key Terms & Strategies | TriumpHealth
- Medicare Billing Guidelines for Q-Codes with CPT 15271–15278: A Guide for Wound Care Physicians
- Why Taxonomy Codes Matter in Provider Credentialing & Medical Billing
- How to Transition Provider Credentialing When Leaving or Joining an ACO
