MIPS FAQ
MIPS Reporting FAQ
1. What is MIPS, and why is it important?
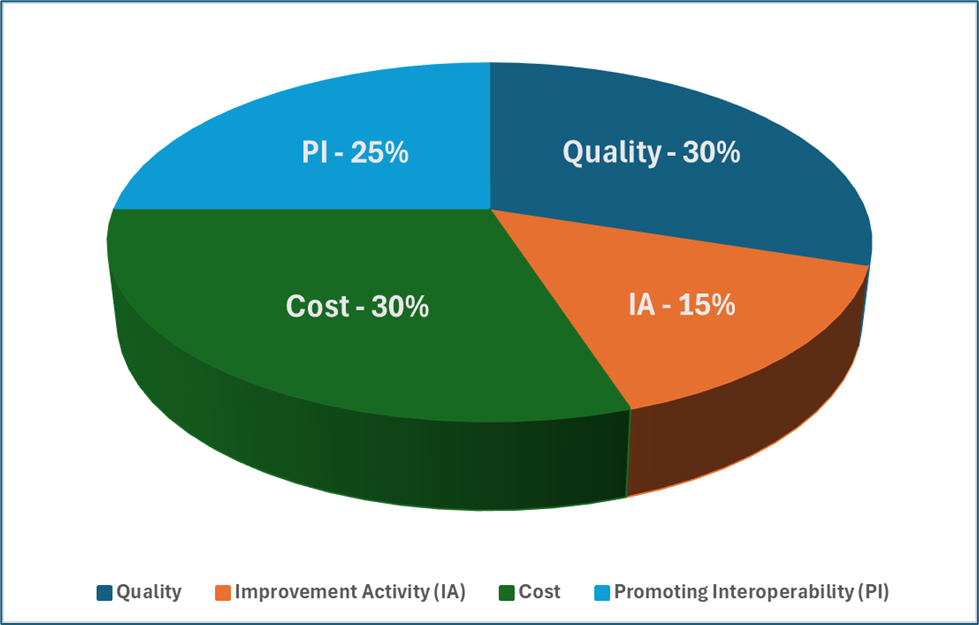
MIPS (Merit-Based Incentive Payment System) is part of the Quality Payment Program (QPP) under Medicare Part B, designed to improve healthcare quality while managing costs. It functions as a value-based care reimbursement model, adjusting Medicare payments based on provider performance in four key categories:
-
-
- Quality (30%) – Clinical performance and patient outcomes.
- Promoting Interoperability (25%) – Use of Electronic Health Records (EHRs).
- Improvement Activities (15%) – Practice enhancements and patient engagement.
- Cost (30%) – Medicare spending efficiency.
-
MIPS participation is essential because it directly impacts Medicare reimbursements, with providers earning incentives for high performance or facing penalties for non-compliance.
2. Who is required to participate in MIPS?
MIPS applies to eligible clinicians who bill Medicare Part B and meet at least one of the following low-volume thresholds:
-
-
- Bill more than a specified amount in Medicare Part B revenue.
- See a set number of Medicare patients.
- Provide a specific volume of Medicare-covered services.
-
Eligible clinicians for MIPS 2025 include:
-
-
- Physicians (MD, DO)
- Nurse Practitioners (NP)
- Physician Assistants (PA)
- Certified Registered Nurse Anesthetists (CRNA)
- Clinical Nurse Specialists
- Groups or Virtual Groups
-
Clinicians below these thresholds may be exempt or have the option to opt-in to earn incentives.
3. What are the key updates for MIPS in 2025?
Performance Thresholds & Scoring Updates
-
-
- The performance threshold remains at 75 points, unchanged from 2023 and 2024.
- Data completeness remains at 75% for all collection types through 2028.
-
Changes in MIPS Performance Categories
Quality Category (30%)
-
-
-
- 196 total measures for 2025.
- Nine new measures added, including two patient-reported outcome measures.
- Eleven measures removed and 66 existing measures updated.
- CMS will introduce flat benchmarking for certain topped-out measures.
-
-
Cost Category (30%)
-
-
-
- Six new cost measures for conditions like respiratory infections and chronic disease management.
- Updates to two existing measures to refine cost tracking.
- A new cost scoring methodology with median-based benchmarking.
-
-
Improvement Activities (15%)
-
-
-
- Two new activities added and two modified.
- Eight activities removed for streamlining.
- Simplified scoring: clinicians attest to one or two activities depending on their practice size and status.
-
-
Promoting Interoperability (25%)
-
-
-
- No major changes, but clinical social workers will no longer receive automatic reweighting.
- Required submission elements include performance data, CMS EHR Certification ID, and attestation details.
-
-
MIPS Value Pathways (MVPs) and Future Transition
-
-
-
- Six new MVPs introduced, expanding specialty-based participation.
- CMS plans to phase out traditional MIPS by 2029, encouraging MVP adoption.
-
-
4. How is MIPS scored, and what are the payment adjustments?
- Providers earn a MIPS score between 0-100 based on their performance in the four categories.
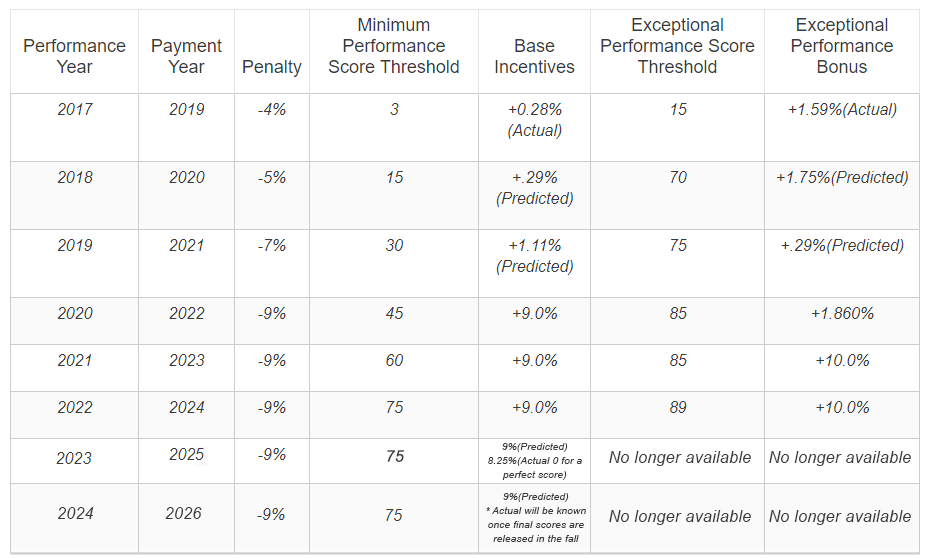
- CMS sets a performance threshold each year:
→ Scores above the threshold earn positive payment adjustments.
→ Scores below the threshold result in negative Medicare payment adjustments (up to -9%).
→ High performers (100 points) may receive a bonus adjustment of around +2%.
5. How do providers report MIPS data?
Clinicians can report MIPS data through:
-
-
- Electronic Health Records (EHRs)
- Qualified Clinical Data Registries (QCDRs)
- Medicare Claims Submission (only for Quality measures)
- CMS Web Interface (for larger groups)
- Qualified Registry Reporting
-
Providers can submit as:
-
-
- Individual clinicians
- Group practices
- Virtual groups
-
Our MIPS compliance consulting helps identify the best reporting method for your practice to maximize scores.
6. What are the key deadlines for MIPS 2025?
-
-
- Performance Year: January 1 – December 31, 2025
- Data Submission Deadline: March 2026
- Payment Adjustment Year: Adjustments for 2025 performance will be applied in 2027
-
7. How can providers optimize MIPS performance and avoid penalties?
To maximize scores and avoid penalties, providers should:
-
-
- Select high-impact Quality measures relevant to their specialty.
- Fully participate in Promoting Interoperability using certified EHRs.
- Choose Improvement Activities that offer the most impact.
- Monitor Cost category performance to adjust spending strategies.
- Use real-time tracking tools to prevent reporting gaps.
-
Our MIPS consultants help providers streamline data collection, submission, and compliance strategies to ensure success.
8. What exemptions and special considerations apply to MIPS?
-
-
- Providers participating in an Advanced Alternative Payment Model (APM) may be exempt from MIPS.
- Hardship exceptions exist for issues like lack of internet access or small practice burdens.
- Performance Category Reweighting is available if data is inaccessible due to third-party issues.
-
Requests for category reweighting must be submitted by November 1, 2025 via the QPP Service Center.
9. How does MIPS compliance consulting help providers?
MIPS compliance consulting helps providers by:
-
-
- Navigating complex MIPS requirements and updates.
- Ensuring accurate reporting and preventing errors that lead to penalties.
- Identifying the best performance measures for maximizing scores.
- Optimizing EHR usage to streamline Promoting Interoperability.
- Providing MIPS audit preparation to ensure compliance.
- Training clinical and administrative teams on documentation and submission best practices.
-
Our consultants stay updated on CMS rule changes and offer personalized guidance to maximize incentives and avoid penalties.
10. How can providers prepare for MIPS 2025?
-
-
- Review eligibility and confirm reporting requirements.
- Select appropriate quality measures aligned with your practice.
- Leverage EHR systems to streamline reporting.
- Monitor performance continuously using dashboards and analytics.
- Engage with Qualified Registries (QCDRs) to simplify data collection and submission.
-
11. How do MVPs (MIPS Value Pathways) impact future reporting?
-
-
- MVPs are designed to simplify MIPS reporting by focusing on specialty-specific performance measures.
- MVPs will eventually replace traditional MIPS by 2029.
- Six new MVPs are being introduced in 2025 for fields like dermatology and urology.
- Clinicians must actively track MVP developments to ensure a smooth transition.
-
12. Can I get professional help with MIPS reporting and compliance?
Yes! Our MIPS consulting services offer:
-
-
- Customized reporting solutions tailored to your practice.
- Expert guidance on measure selection and compliance strategies.
- Assistance with data collection and submission to avoid penalties.
- Audit preparation support to maintain compliance.
-
By staying informed on CMS regulations, TriumpHealth helps providers navigate MIPS changes and maximize reimbursement opportunities. For additional questions, please contact us at [email protected] or (888) 757-3836.
Maximize Your Revenue. With Expert RCM Services
Schedule a consultation today to achieve financial success and regulatory compliance. Let us help you improve patient outcomes while increasing your revenue.


