MIPS Reporting Made Easy: 8 Steps to Understand MIPS Scoring | TriumpHealth
MIPS Reporting Made Easy: 8 Steps to Understand MIPS Scoring | TriumpHealth
The Merit-Based Incentive Payment System (MIPS) was established under the Quality Payment Program (QPP) as part of the Medicare Access and CHIP Reauthorization Act (MACRA) and came into effect on January 1, 2017. MIPS is one of three tracks under the QPP, alongside MIPS Value Pathways (MVP) and Advanced Alternative Payment Models (Advanced APMs). Eligible clinicians (ECs) earn a performance-based payment adjustment, applied to their Medicare payments two years after the performance year. In 2025, MIPS has undergone significant changes, making it one of the most challenging years for participants.
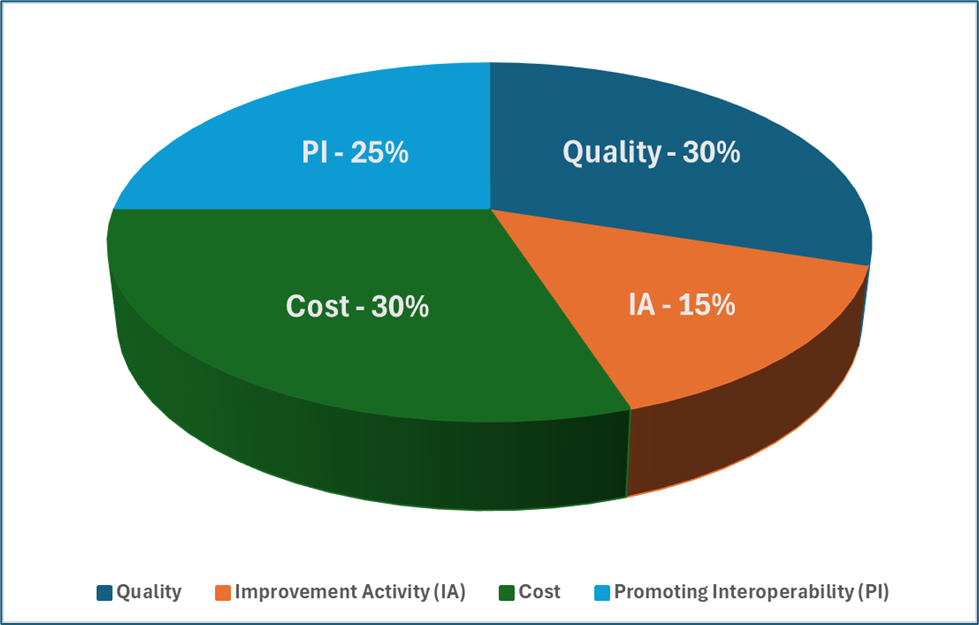
Key Performance Categories and Weights for 2025
MIPS scores are calculated based on four performance categories:
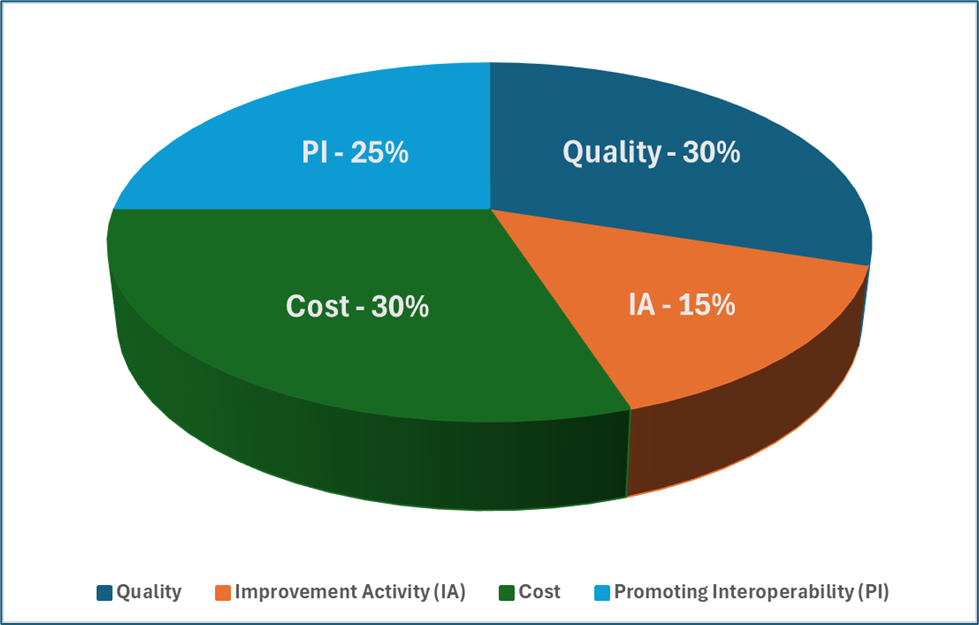
These categories combine to form a score out of hundred (100). To avoid penalties, a minimum threshold of seventy-five (75) points is required. Meeting these benchmarks involves stringent reporting and compliance with category-specific requirements.
Steps to Calculating MIPS Scores
Step 1: Reporting Models
Clinicians can participate in MIPS through different reporting methods:
- Individual Reporting: Tied to a specific NPI and TIN combination, where each clinician’s score is based on their data.
- Group Reporting: All eligible clinicians within a shared TIN are scored collectively.
- Virtual Groups: Similar to group reporting but allows clinicians from different TINs to participate together.
- Facility-Based Reporting: Allows clinicians to use facility performance scores for Quality and Cost categories.
- MIPS-APM Reporting: Utilizes the APM Scoring Standard for participants in Advanced Payment Models not meeting QP thresholds.
- MVP Reporting: Specialty-specific pathways aimed at reducing reporting burdens while maintaining compliance.
Step 2: Quality Measures and Data Requirements
Clinicians must report data for six (6) measures when reporting through the traditional MIPS track, including for Individual, Group, Virtual, and APM reporting. Quality measures need to be tracked and documented over a full calendar year. Data completeness (75%) and case minimums (20 cases) are critical. New measures meeting completeness requirements receive seven points.
When reporting through an applicable MVP, clinicians must report four (4) Quality measures but those measures need to come from the set of measures under that specific MVP.
For instance, if there was an individual clinician reporting through traditional MIPS, they could choose any six (6) measures (either available through the EHR, applicable registry, or some combination). If the clinician were to participate in the Advancing Cancer Care MVP, then they must choose four (4) measures from that MVPs list of measures.
Step 3: Quality Score Calculation
Achievement points are capped at ten (10) per measure, with a total of 60 potential points for six measures. Small practices receive a six-point bonus in this category. Improvement in Quality scoring from the previous year can potentially add up to 10 percentage points.
Step 4: Promoting Interoperability (PI) Exclusions and Exceptions
The PI category evaluates the use of certified electronic health record technology (CEHRT). Changes for 2025 include a mandatory reporting period of one hundred and eighty (180) continuous days. Certain clinicians, such as those in small practices or non-patient-facing roles, may qualify for automatic reweighting.
Step 5: Promoting Interoperability Scoring
Scoring is based on objectives such as e-Prescribing, Health Information Exchange, Provider-to-Patient Exchange, and integration with Public Health registries in your state. Bonus points are available for reporting on additional public health measures. A maximum of hundred (100) points is possible, translating to 25% of the final score.
Step 6: Improvement Activities (IA)
The IA category incentivizes care coordination, patient engagement, and safety initiatives. In 2025, small practices, rural practices, and non-patient-facing clinicians only have to report one Improvement Activity while large practices must attest to two Improvement Activities. Data must be reported for at least ninety (90) continuous days, and full credit is possible with forty (40) points.
A minimum of 50% of clinicians in a group must perform the same activity for it to count.
Step 7: Cost Category
The Cost category, weighted at 30%, requires no data submission during attestation as CMS calculates scores using administrative claims data received for patient visits during the reporting year. There are 29 measures divided into procedural, acute inpatient, and chronic condition-based categories.
Step 8: Final MIPS Score Calculation
Final scores are calculated by combining weighted scores from all categories. Reweighting may occur if a category cannot be scored (do not meet the case minimum for a Cost measure), or if the PI category automatic reweight was kept in place by a small practice, or if there is an approved hardship in place. Up to 10 bonus points may be awarded by CMS for treating complex patients.
Payment Adjustments
Based on their 2025 performance, clinicians may receive a payment adjustment ranging from -9% to +9% in payment year 2027. Scores below 18.75 incur the maximum penalty, while scores between 75.01 and 100 earn scaled positive adjustments.
Special Considerations for Small Practices
Clinics with 15 or fewer clinicians have unique advantages:
- A six-point bonus in the Quality category.
- Automatic reweighting for PI unless data is submitted.
- Three points for Quality measures not meeting data completeness requirements.
Conclusion
Navigating the complexities of MIPS can be challenging, especially with the evolving requirements and performance thresholds. TriumphHealth offers comprehensive MIPS consulting services designed to help clinicians and practices optimize their performance in all categories. By leveraging expert guidance, practices can ensure accurate reporting, meet compliance standards, and maximize their MIPS scores. Visit TriumpHealth to learn how their tailored solutions can help your practice succeed in the MIPS program.
Disclaimer:
The content provided by TriumpHealth is for informational purposes only and does not constitute legal, medical, or financial advice. Regulations and payer requirements may change; please consult a qualified professional for guidance specific to your situation. Click here to review our full legal disclaimer.
Recent Posts
- MIPS 2026 Quality Performance Category: Understanding Collection Types and Reporting Strategies
- MIPS 2026 Updates: A Practical Guide for Clinicians, Practices, and Office Managers
- CHAP Accreditation Updates for DME Suppliers: Step-by-Step Guide for Location Changes and Adding New DME Supplies
- Payer Contract Negotiations: Key Terms & Strategies | TriumpHealth
- Medicare Billing Guidelines for Q-Codes with CPT 15271–15278: A Guide for Wound Care Physicians
- Why Taxonomy Codes Matter in Provider Credentialing & Medical Billing
