Six Proactive Medical Billing Tips to Maximize Revenue | TriumpHealth
Six Proactive Medical Billing Tips to Maximize Revenue | TriumpHealth
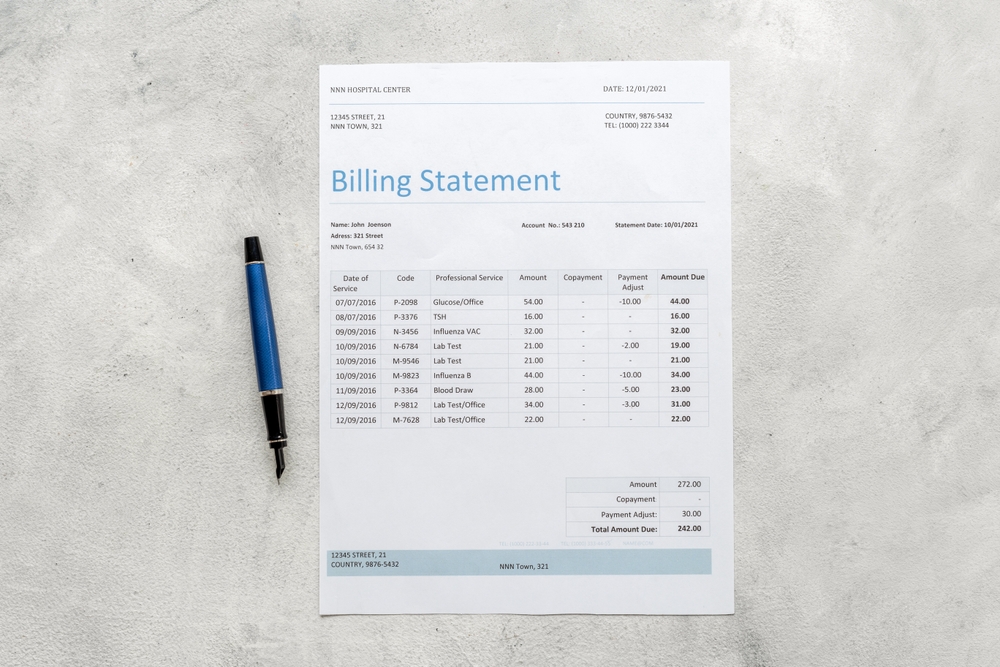
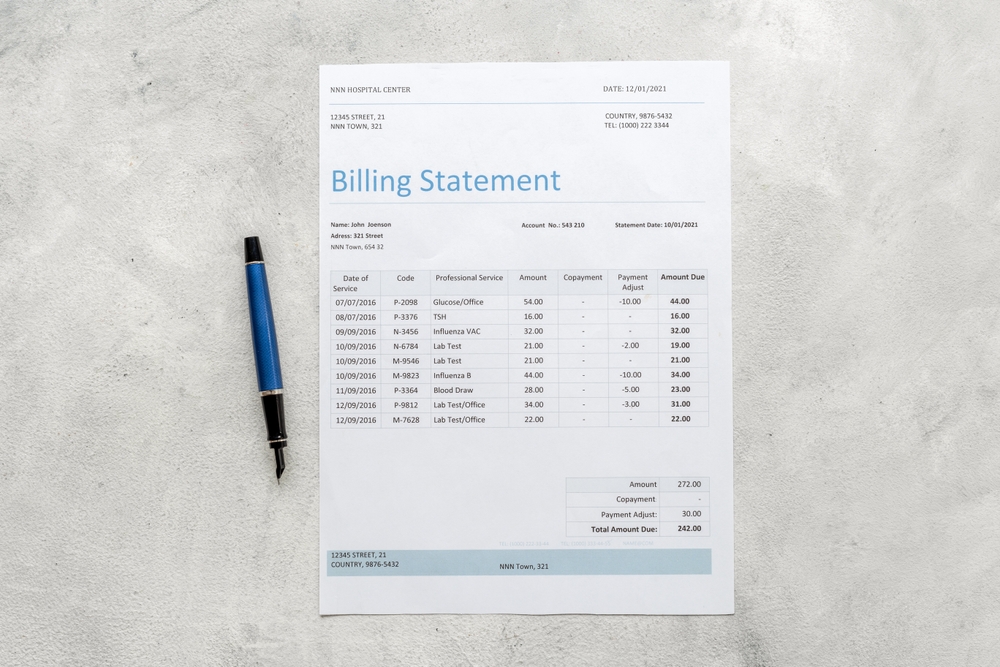
Continuous changes in the U.S. healthcare system create challenges for providers and patients. Healthcare reform complicates billing, such as adopting more time-consuming, value-based compensation models. Frequent billing rules and regulations changes can lead to revenue losses for healthcare providers nationwide. Consequently, the failure to stay up-to-date on medical billing rules and billing errors results in significant uncollected revenue each year.
Overcoming Financial Hurdles: Proactive Medical Billing Strategies
Despite these challenges, healthcare providers can find hope. Medical practices can reduce financial losses by taking a proactive approach to medical billing processes. They can also mitigate compliance risks and maximize revenue. Here are six proactive steps your healthcare practice can take to optimize medical billing procedures:
- Establish a Streamlined Collections Process
To ensure the financial health of your practice, establish a straightforward collections process. This process should clarify responsibilities for all parties involved. Moreover, it should improve revenue cycles by ensuring patients understand their financial obligations.
Key Steps:
- Clearly Define Payment Expectations: Communicate payment expectations to patients through initial paperwork and ongoing reminders. This communication helps prevent confusion about their obligations.
- Gather Comprehensive Patient Information: Collect detailed and up-to-date contact information, including photo IDs. This information facilitates follow-up on outstanding payments.
- Regularly Update Contact Information: Ensure you have the correct addresses and phone numbers. This practice avoids the inefficiencies of chasing incorrect leads.
- Obtain Message Permissions: Secure patient consent to leave billing-related messages on voicemail. This step streamlines communication.
Emphasize Co-pay Reminders: Consistently remind patients about their co-pays. Ensure your staff is prepared to address any related questions. - Verify Insurance Eligibility Frequently: Use automated systems to verify insurance eligibility regularly. This practice reduces the risk of claim denials.
- Request Payments Upfront: Collect co-pays and outstanding balances before services are rendered. This strategy minimizes future collection efforts.
- Offer Flexible Payment Options: Provide clear information about payment methods and plans. This approach makes it easier for patients to meet their obligations.
- Send Timely Payment Reminders: Implement a sequence of reminder letters. This ensures patients are aware of upcoming, overdue, or collections-bound bills.
- Optimize Claims Management
To ensure timely and accurate reimbursement, optimize your claims management process. By submitting clean, error-free claims from the start, you can avoid costly corrections and delays in payment.
Key Strategies:
- Ensure Accurate Data Entry: Double-check that all patient and provider information is accurate and complete. This step helps avoid common errors that lead to rejections.
- Verify Insurance Details: Confirm that insurance information, including policy numbers and payer IDs, is correct and up-to-date. This verification prevents unnecessary claim denials.
- Prevent Duplicate Billing: Implement checks to ensure services are billed only once. This practice avoids the pitfalls of duplicate submissions.
- Enhance Clinical Documentation Quality: Work closely with providers to document all procedures thoroughly. This effort reduces the likelihood of errors that could delay claim approval.
- Follow-up on Submitted Claims: Maintain regular communication with insurance companies. This communication helps track the status of submitted claims and quickly addresses any issues.
- Review Denial Codes and EOBs: Carefully examine the Explanation of Benefits (EOBs) and denial codes when claims are rejected. Reach out to the payer for clarification before resubmitting.
By optimizing your claims management process, you can significantly reduce the time spent on corrections. This approach ensures a smoother, more efficient revenue cycle for your practice.
- Minimize Coding Errors
Accurate medical coding ensures proper reimbursement and avoids claim denials. By enhancing coding accuracy, your practice can reduce errors and maximize revenue.
Key Approaches:
- Strengthen Notes Documentation Practices: Ensure providers document procedures with detail, especially under ICD-10 requirements. This practice supports precise coding and reduces non-specific diagnosis codes.
- Use Appropriate Modifiers: Pay close attention to modifier usage, especially in specialties like radiology. Verify that all necessary modifiers are included and correctly applied based on payer requirements.
- Avoid Upcoding and Undercoding: Double-check codes to prevent accidental or intentional upcoding or undercoding. Clear communication between coders and providers accurately reflects the services rendered.
- Leverage Coding Resources: Utilize up-to-date coding manuals, software, and resources to assign correct codes. Cross-checking with reliable coding tools helps avoid common mistakes.
- Provide Ongoing Training: Regularly train your coding staff on the latest coding guidelines and payer-specific rules. This training keeps them informed and minimizes errors.
By focusing on coding accuracy, you can significantly decrease the likelihood of claim rejections and denials. This leads to a more efficient revenue cycle and better financial outcomes for your practice.
- Expedite Resolution of Denied and Rejected Claims
Effectively managing denied and rejected claims is vital for maintaining cash flow. Promptly addressing these issues can minimize payment delays and improve overall revenue cycle efficiency.
Key Actions:
- Differentiate Between Denied and Rejected Claims: Understand the distinction between denied claims (processed but unpaid) and rejected claims (not processed due to errors). This knowledge helps determine the appropriate corrective action.
- Act Quickly on Rejections: Correct and resubmit rejected claims immediately. Ensure you address all identified errors before resubmission to avoid further rejections.
- Appeal Denied Claims: For denied claims, initiate the appeal process promptly. Gather all necessary documentation and communicate with the payer to clarify the reasons for denial.
- Maintain Open Communication with Payers: Regularly contact payer representatives to discuss problematic claims. Seek clarifications and stay aware of changes in processing guidelines.
- Track and Analyze Denials: Monitor trends in denied and rejected claims to identify recurring issues. Use this data to implement process improvements.
By expediting the resolution of denied and rejected claims, you can reduce the time and resources spent on corrections. This practice leads to faster reimbursement and a more efficient billing process.
- Commit to Continuous Improvement
In the ever-evolving healthcare landscape, continuous improvement is essential for maximizing revenue. By regularly evaluating and refining your processes, your practice can stay ahead of challenges.
Key Initiatives:
- Monitor Financial Metrics: Regularly track key performance indicators such as accounts receivable and claim denial rates. Analyze these metrics to identify trends and assess the effectiveness of current practices.
- Stay Updated on Industry Changes: Keep your team informed about the latest medical billing regulations and payer requirements changes. This knowledge may involve ongoing education and training sessions.
- Implement Feedback Loops: Encourage staff to share insights and suggestions for improving billing processes. Regularly review and act on this feedback to foster a culture of continuous improvement.
- Adopt Best Practices: Research and integrate industry best practices into your workflows. Stay connected with professional networks to learn from others’ experiences.
- Invest in Technology: Leverage advanced billing and coding software to automate repetitive tasks. Regularly assess your technology needs to ensure your practice has the best tools.
By committing to continuous improvement, your practice can adapt to changes and enhance operational efficiency. This approach ensures long-term success in a dynamic healthcare environment.
- Recognize When to Outsource Your Medical Billing
Balancing patient care, administrative tasks, and staying current with industry regulations can overwhelm any medical practice. Knowing when to outsource billing functions can significantly improve efficiency.
Key Considerations:
- Assess Workload and Resources: Evaluate whether your in-house team has the time and expertise to manage billing effectively. If your staff is frequently overwhelmed, consider outsourcing.
- Analyze Cost-Benefit: Compare the costs of maintaining an in-house billing department with outsourcing. Factor in expenses related to training and potential errors that lead to lost revenue.
- Identify Specialized Needs: Certain specialties, such as radiology or pathology, require specialized billing knowledge. If your practice struggles in these areas, outsourcing can ensure accuracy.
- Focus on Core Competencies: By outsourcing non-core tasks like billing, your practice can dedicate more resources to patient care. This shift enhances overall productivity.
- Evaluate Outsourcing Partners: When selecting an outsourcing partner, choose a company with a proven track record. Ensure they stay updated on industry changes and provide the service your practice requires.
Managing a medical practice involves staying current with coding standards and billing regulations. When the burden becomes too great, consider outsourcing to specialized companies.
Benefits of Outsourcing:
Outsourcing medical billing and coding offers several strategic benefits. These benefits can help your practice streamline operations and enhance financial performance:
- Expertise at Your Fingertips: Outsourcing provides access to professionals who specialize in billing and coding. Their expertise reduces the likelihood of errors and improves claim processing speed.
- Cost Efficiency: By outsourcing, you can save on overhead costs related to hiring and training an in-house team. This approach eliminates costs for software and office space.
- Faster Revenue Cycles: Outsourced billing companies focus on processing claims, leading to quicker submissions and faster reimbursements. This result improves cash flow.
- Scalability: An outsourcing partner can quickly scale their services as your practice grows. This flexibility allows you to meet changing needs without additional staff.
- Focus on Patient Care: With the administrative burden lifted, your staff can concentrate on delivering quality patient care. This focus leads to higher patient satisfaction and better health outcomes.
- Regulatory Compliance: Outsourcing firms stay current with industry changes and compliance requirements. This practice helps your practice avoid costly errors and penalties.
Outsourcing your billing and coding functions can enhance efficiency and reduce costs. This approach strengthens the financial foundation for your practice.
Partner with the TriumpHealth Medical Billing Team
Streamline your medical billing with TriumpHealth. Our expert team specializes in revenue cycle management for medical specialty practices, ensuring you receive the full revenue you deserve.
With TriumpHealth, you can enhance cash flow, reduce operational costs, and stay compliant with industry regulations. We take care of the complexities of billing, allowing you to focus on patient care. If you’re facing overdue accounts or unresolved claims, contact us today at (888) 747-3836 x0 or [email protected] and discover how our outsourced medical billing services can optimize your practice’s financial health.
Disclaimer:
The content provided by TriumpHealth is for informational purposes only and does not constitute legal, medical, or financial advice. Regulations and payer requirements may change; please consult a qualified professional for guidance specific to your situation. Click here to review our full legal disclaimer.
Recent Posts
- MIPS 2026 Updates: A Practical Guide for Clinicians, Practices, and Office Managers
- CHAP Accreditation Updates for DME Suppliers: Step-by-Step Guide for Location Changes and Adding New DME Supplies
- Payer Contract Negotiations: Key Terms & Strategies | TriumpHealth
- Medicare Billing Guidelines for Q-Codes with CPT 15271–15278: A Guide for Wound Care Physicians
- Why Taxonomy Codes Matter in Provider Credentialing & Medical Billing
- How to Transition Provider Credentialing When Leaving or Joining an ACO
