Provider Credentialing
Services
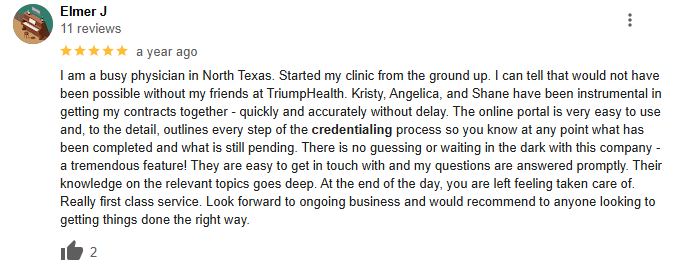
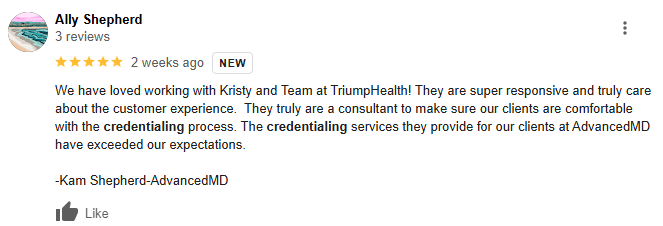
TriumpHealth simplifies provider credentialing, ensuring fast insurance enrollment so healthcare professionals can focus on increasing revenue and improving patient care.
Credentialing with insurance companies is a vital step in ensuring that healthcare providers and organisation are eligible for reimbursement from health insurance plans. This process verifies provider qualifications and eligibility, allowing you to build a network of trusted payers and ensure you’re compensated for your services.
We work with you to ensure the credentialing process is as efficient as possible, helping you navigate the complexities of insurance companies and securing partnerships with major payers.
At TriumpHealth, we offer a full suite of services tailored to your credentialing and payer enrollment needs. Our expert team simplifies the process so you can focus on what matters most: providing excellent patient care.

CAQH (Council for Affordable Quality Healthcare) registration is a key component of the credentialing process. We help healthcare providers complete and maintain their CAQH profiles, ensuring that you’re ready to be credentialed by multiple insurance payers with a single, streamlined application process.

Maintaining your credentialing and payer enrollment status is just as important as the initial application. We offer ongoing monitoring and support to ensure your credentials remain active and you continue to meet all compliance requirements for insurance companies.

For healthcare providers who serve Medicare and Medicaid patients, our enrollment services ensure compliance with all federal regulations. We assist with the application process and work with you to maintain active enrollment status.

Payer enrollment is the process of enrolling with insurance carriers and government programs. Our team ensures that your information is accurately submitted to insurance companies and health plans, helping you get listed as a participating provider in a timely manner.

Primary source verification is a crucial step in confirming a provider’s qualifications, including education, licensure, and work experience. We manage this process to ensure your credentials meet the necessary standards and are verified directly from the original sources.

We manage the entire provider credentialing process—from CAQH registration to application completion, audit, follow up and Payer approval—so you don’t have to do it. Our proven workflows reduce delays and increase your approval rates, saving you time and hassle.

We offer full-service credentialing, including primary source verification, payer enrollment, and Provider Credentialing maintenance. With us, you’ll have one trusted partner handling everything to ensure continuous compliance and enrollment.
Data collection of all legal, financial, and organizational documents from providers and organizations for application filing and submission with private, commercial & government payers.
Complete reconnaissance of current provider enrollment status. Submit applications with desired payers and complete timely follow-ups with payers to track application statuses.
Receive a countersigned copy of the contract and/or verify that the provider has in-network participation with written confirmation from the desired payer.
TriumpHealth is here to ensure that your office obtains its credentials accurately and on time so that you can begin receiving reimbursement as soon as possible. Missed deadlines and incorrect documentation cause an already time-consuming process to become a nightmare. We have the experience and knowledge you need to get you through the process with the least amount of worry. Your office simply needs to provide us with the required information and documents – and then leave the heavy lifting for us!
Provider Credentialing and Payer Enrollment

We handle meticulous process of verifying documentation to ensure you can deliver care without hold-ups.

With ongoing oversight, we keep your credentials up to date and in compliance with all regulatory requirements, guaranteeing uninterrupted revenue.

Offload the administrative burden from your staff to us, allowing you to focus on day-to-day operations.

Gain access to a broad range of payer networks, increasing your patient reach and revenue.
Contact TriumpHealth today to learn more about our comprehensive provider credentialing services and how we can support you.
By clicking ‘Submit,’ you agree to TriumpHealth’s Terms Of Service and TriumpHealth’s use of the information you have provided in accordance with our Privacy Policy.
Additionally, you agree to receive promotional phone calls or text messages from TriumpHealth at the phone number provided. Message and data rates may apply. You can STOP messaging by sending STOP and get more help by sending HELP.
Schedule a consultation today to achieve financial success and regulatory compliance. Let us help you improve patient outcomes while increasing your revenue.
Fill out the form below and we’ll get back to you shortly.
