AI in Prior Authorization: Speeding Approvals & Improving Patient Care

AI in Prior Authorization: Speeding Approvals & Improving Patient Care
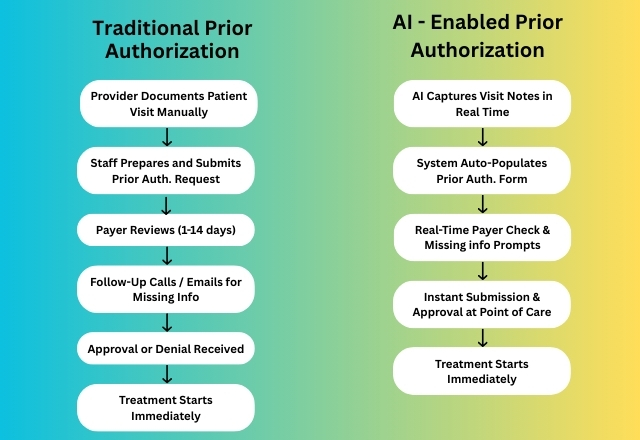
Prior authorization has historically been one of healthcare’s most time-consuming administrative processes, often taking days or even weeks to secure approvals for medically necessary treatments. These delays frustrate patients, increase clinician workload, and can result in postponed or abandoned care.
Today, artificial intelligence (AI) is emerging as a game-changer, enabling healthcare organizations to process prior authorizations in real time during patient encounters.
AI’s Role in Revolutionizing Prior Authorization
1. Automated Documentation Capture
AI can listen, transcribe, and summarize patient visits into structured clinical notes. This removes the need for after-hours charting and ensures that documentation is complete and compliant with payer requirements.
2. Real-Time Data Validation
AI algorithms can instantly check payer rules and guidelines, prompting providers for any missing information during the patient visit, avoiding back-and-forth communications and rework.
3. Instant Submission and Decision Support
Integrated AI tools can auto-populate prior authorization forms, attach relevant clinical documentation, and submit them directly to payers. In some cases, approvals can be obtained before the patient leaves the office.
Key Benefits of AI-Driven Prior Authorization
- Faster Access to Care
Real-time approvals mean patients start treatment sooner, improving outcomes and satisfaction. - Reduced Clinician Burnout
By eliminating repetitive administrative work, AI gives providers more time to focus on patient care. - Improved Accuracy & Compliance
AI helps ensure that submissions meet payer requirements the first time, reducing denials. - Lower Administrative Costs
Streamlining prior authorization reduces manual labor, phone calls, and follow-ups.
Best Practices for Implementing AI in Prior Authorization
- Integrate AI into Your EHR so it works within the provider’s existing workflow.
- Use Clinical Intelligence to passively capture and structure data.
- Prioritize Security and HIPAA Compliance to protect patient information.
- Train Staff on how to interact with AI prompts and use real-time feedback to improve efficiency.
Conclusion
AI is reshaping the prior authorization process from a slow, paper-heavy bottleneck into a streamlined, real-time decision-making tool. By integrating AI into clinical and administrative workflows, healthcare organizations can improve patient care timelines, reduce operational costs, and alleviate the administrative burden that has long contributed to clinician burnout.
Ready to streamline your Prior Authorization and revenue cycle process? Schedule a consultation today or contact us at [email protected] or (888) 747-3836 x0, to learn how our credentialing and revenue cycle experts can help your prior authorization-speeding approvals & improving patient care.
Disclaimer:
The content provided by TriumpHealth is for informational purposes only and does not constitute legal, medical, or financial advice. Regulations and payer requirements may change; please consult a qualified professional for guidance specific to your situation. Click here to review our full legal disclaimer.
Recent Posts
- MIPS 2026 Updates: A Practical Guide for Clinicians, Practices, and Office Managers
- CHAP Accreditation Updates for DME Suppliers: Step-by-Step Guide for Location Changes and Adding New DME Supplies
- Payer Contract Negotiations: Key Terms & Strategies | TriumpHealth
- Medicare Billing Guidelines for Q-Codes with CPT 15271–15278: A Guide for Wound Care Physicians
- Why Taxonomy Codes Matter in Provider Credentialing & Medical Billing
- How to Transition Provider Credentialing When Leaving or Joining an ACO